The Medicare Advantage (MA) program has expanded rapidly and now accounts for more than half of total Medicare enrollment. However, as the program grows, its payments for services have continued to shrink. In fact, their payments for services rendered have gotten so low that more and more rural hospitals have stopped accepting their coverage altogether.
In the past decade alone, more than 100 rural hospitals have closed in the U.S. and more than 400 are in high financial risk. In addition, data shows that MA pays less than Medicare, which is also cited for paying less than cost of care. (Chart right) Next, 81% of providers report that MA patients require more paperwork, insurance requirements, and longer wait times for services. That accounts for 9.6% longer wait times for care than traditional Medicare patients. (Data from American Hospital Association)
This year alone, 32 large health systems have dropped their MA contracts, though no official number on rural hospitals has been collected. However, a survey showed that out of 135 health system CFOs, 16% were dropping MA contracts and another 45% were considering the same. (Data from Becker’s Hospital Review)
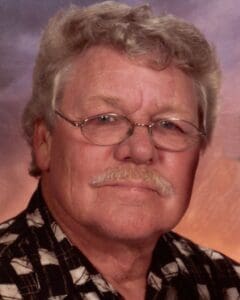
The Local Take
As of January 1, 2025, Clay County Medical Center no longer accepts Medicare Advantage.
CCMC Revenue Cycle Director, Sharla Shivers, CSPR, CRCR, explained the process of accepting medical insurance and why the facility updated its coverage options.
Shivers is a Certified Revenue Cycle Representative and Certified Specialist Payment and Reimbursement rep and has worked with the company for seven years.
Why did CCMC stop accepting Medicaid Advantage?
“Medicare Advantage plans continue to put obstacles between the patient and their medical provider for care planning and decision making. In some cases, it denies or at least delays care past the point of safety. We did not want to add stress to patients enrolled in these plans: the restrictions the plans put on their patients and the facilities that are trying to take care of them is no longer something we felt was acceptable. It also allows patients to have an expectation of the amount due for services instead of being surprised by a bill for services they expected would be covered by their plan but were not.”
“In addition, CCMC does not accept out-of-state Medicaid, Christian health share plans, or any coverage that follows a primary Medicare Advantage plan.”
How do insurance payments work?
“Claims are sent to insurance companies for processing. Those companies then send processing results back to us on remits along with any applicable payments. These remits tell us what was processed and covered by the plan as well as any services that were denied by the plan guidelines and the reason for that denial. Our billing staff then reviews all denials to see if there is anything we can appeal to increase the coverage for the patient’s visit. We appeal those denials with medical records and/or peer-to-peer phone calls between the provider and the insurance plan, depending on the insurance plan rules. The plan then reviews the appeal and processes the claim again. This either results in a change to the coverage determination or the original denial is upheld. If the original denial is upheld, we may have other options for appeal depending on the insurance plan. Once all options for appeals are exhausted, anything the insurance does not pay for and was not designated as patient responsibility is written off.
“Because Medicare pays private insurance companies that offer Medicare Advantage plans a fixed amount per month, when patients stay healthy, that private company keeps those funds. If the beneficiary has any services done, the private company must utilize that fixed amount to pay for care. This arrangement allows private insurance companies to micro-manage a patient’s care to protect those fixed amounts. In addition, Medicare stays stable year to year, while Advantage plan benefits can change annually and come with unexpected out-of-pocket costs, which is difficult for those on a fixed income.”
What is the average payment timeline for a service?
“Payment timelines vary based on the insurance plan. Medicare, BlueCross, and other large commercial payers process fairly quickly for initial claims, usually within 2-4 weeks of submission. Other payers can take longer for initial processing, sometimes they can take months to pay. Any appeals needed will add several weeks to that processing time, regardless of payer.”
How does insurance payment affect the hospital?
“The quicker the payment is received from the insurance and the fewer submissions it
requires to get the insurance to process charges correctly, the lower the administrative
burden is on the facility. The billing department’s job is to make sure the insurance is
paying for all the services the patients’ plan mandates as well as make sure the hospital
is receiving the correct reimbursement for those services based on our contracts with the plan.”
If a patient is unhappy with their Medicare or private medical insurance, Shivers said they can call SHICK (senior health insurance counseling for Kansas). The SHICK program is a branch of the Kansas Department of Aging and Disability Services and can be reached at 800-860-5260.