by Bethaney Phillips
On February 5th, many local pharmacies will close as their employees head to Topeka to speak with lawmakers. Through the Kansas Pharmacists Association, they will discuss a potential reform to reign in the way prescriptions are currently sold and billed.
Currently in Kansas, prescriptions and their prices are almost exclusively regulated by PBMs, Pharmacy Benefit Managers. According to local pharmacists, there are multiple aspects that need to be adjusted with a reform.
“The biggest issue is transparency, we should see the details,” said pharmacist Brandon McCune, who has been a pharmacist since 2013.
During this Advocacy Day, McCune, who works at Ferguson-Rexall in Clay Center, and others will join the conversation with Kansas lawmakers. PBM regulation (or lack thereof) is managed at the state level, leaving room for interpretation. McCune said he previously worked in Oklahoma, where laws limit what PBMs can do and charge.
Pharmacists from Patterson’s in Clay Center, along with their other five locations, will also be also in attendance. Though they will open at 1 pm, to avoid inconveniencing customers, they fear that could be the norm – a lack of pharmacy – if the status quo doesn’t change.
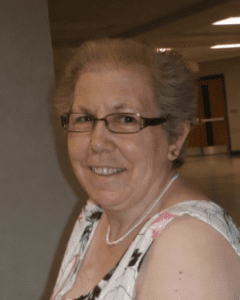
“In the past three or four years there has been a drastic drop in payments to us,” said pharmacist Roxie Martin, “Some are what they call completely underwater on claims.”
Recently, Martin, who’s been a pharmacist for 30 years, said she filled a prescription where the patient paid $.15 and insurance paid $0.
“We can’t even buy the medicine bottle for that, let alone add a label, our time, plus the medicine in the bottle,” she said. “I’m all for inexpensive medication, but this is just ridiculous. There should be a minimum price for a professional service.”
Issues Kansas Pharmacies are Addressing:
-Three big PBMs manage the majority of pharmacy negotiations: CVS Caremark (CVS/ Aetna), Express Scripts (Cigna), and OptumRx (UnitedHealth Group)
-PBMs negotiate rebates that lower prices of drugs, dropping them on a tier rate, which can get them prescribed more often. Rather than passing the rebate savings to consumers, PBMs keep the undisclosed funds as profit, while relaying to insurance companies and lawmakers that they have lowered prescription costs.
“Our issue with the rebate is it’s completely invisible, no one knows what these rebates are but what we do know is that the profit margins and revenues are very, very high,” said McCune. “They’re actually raising the cost of healthcare for everyone involved.”
-PBMs often pay pharmacies less for medications than it cost the pharmacy to get the drug, forcing them to take a loss. The way it’s negotiated, PBMs also pay less to smaller pharmacies, meaning those owned by PBMs take a larger cut per-pill for the same prescription as an independently owned location.
“It’s a way for them to squeeze us and put us out of business,” McCune said. “Three out of five independent pharmacies have closed. It’s working, they’re very good at what they’re doing.”
After checking with the Kansas Pharmacy Association, Martin relayed that two independent Kansas pharmacies have closed this year, while another 10 closed in 2024. Since 2016, a total of 52 have closed.
“That’s a lot,” Martin said. “It’s kind of scary for independent pharmacies.”
-Mail-order steering, or requiring patients to get refills from a mail-order company, rather than a local pharmacy, is common practice. Because the PBMs own major health insurance companies and pharmacies, prescriptions are steered toward their own facilities, rather than a pharmacy picked by geographic location or patient choice.
Martin said recently a patient called in, relaying that her mail-order prescription was delayed by three weeks before she was notified it couldn’t be filled.
“It was mandatory for her to have mail-order, then after the wait they wanted us to fill it,” she said. Adding that the pharmacy did fill the prescription, albeit at a loss. “Forcing mail order has gotten worse in the last five years.”
-Every prescription goes through a “data switch,” including patient information like name, date of birth, address, doctor prescribing, and more. There are two main data switches and both are owned by United. This could potentially give key information on prescriptions and patients to control the market.
“Plan sponsors need to know more about PBM rebates and their spread pricing,” McCune said.
-PBMs have one of the largest lobbying groups in the country, spending $15 million in 2023, second only to pharmaceutical researchers and manufacturers. This was after spending $8.6 million in 2022; $8.4 million was spent in the first half of 2024 alone.
In addition, he said it should be the patient’s choice as to where they get their medication, not be forced to an online service.
“We are advocating for increased transparency, protection against mail-order steering, and overall better prices for our patients,” he said. “That’s why we’re going and we’ll have a meeting at the Capitol and go over some talking points with our lawmakers to discuss some of these issues for them.”
A form letter is also available for patients and pharmacy customers to share past issues, or why having a local pharmacy is important.